
CINCINNATI, Feb. 22, 2017 /PRNewswire-USNewswire/ -- Scientists propose in Nature blocking a molecule that drives inflammation and organ damage in Gaucher and maybe other lysosomal storage diseases as a possible treatment with fewer risks and lower costs than current therapies.
An international research team led by Cincinnati Children's Hospital Medical Center, which also included investigators from the University of Lübeck in Germany, report their data Feb. 22. The study was conducted in mouse models of lysosomal storage disease and in cells from blood samples donated by people with Gaucher disease.
Current treatments for Gaucher and other lysosomal storage diseases (LSDs) include enzyme replacement therapy or substrate reduction therapy. These break down or prevent the accumulation of certain fatty molecules and other waste particles that clog cells to cause inflammation, cell and organ damage and, in some cases, death. People with LSDs lack enzymes that break down used-up proteins and other spent particles, preventing their cells from shedding these waste materials and functioning normally.
Individually, the 50 genetic diseases characterized as LSDs are considered rare. But collectively they have a frequency of one in 8,000 births, making LSDs a major challenge for the health care system, according to information from the National Institutes of Health. Study authors stress there is a need for new therapies.
"Current enzyme replacement and substrate reduction therapies are expensive and still associated with inflammation, increased risk of malignancies and Parkinson's disease," says Manoj Pandey, PhD, study first author and a scientist in the Division of Human Genetics at Cincinnati Children's. "We suggest that targeting a molecule called C5aR1 may serve as a viable treatment option for patients with Gaucher disease and possibly other LSDs."
Pandey is co-corresponding author on the paper along with Jörg Köhl, MD, director of the Institute for Systemic Inflammation Research at the University of Lübeck, and adjunct professor in the Division of Immunobiology at Cincinnati Children's.
Finding a target
In laboratory mouse models and human cells, researchers show that C5aR1 is a critical part of a molecular pathway that drives pro-inflammatory processes in Gaucher disease, which is initiated by mutations of a gene known as GBA1. GBA1 encodes the lysosomal enzyme glucocerebrosidase (GCase), which degrades the fatty molecule glucosylceramide (GC). C5aR1 is a receptor for a small peptide (a protein component) that is derived from the complement system (part of the immune system) called C5a, which drives inflammation in several different types of immune cells.
The disease process starts by GBA1 mutation driving extensive accumulation of glucosylceramide in immune cells. Before the current study, the molecular process that connects glucosylceramide accumulation to inflammation was unknown, as was the role of inflammation in disease development.
Pandey and colleagues show inflammatory glucosylceramide accumulation in spleen, liver, lung and bone marrow immune cells in Gaucher mouse models drives the induction of auto-antibodies against glucosylceramide, which form immune complexes. These immune complexes promote the production of C5a and activation of its receptor C5aR1.
In organ tissues from disease mouse models, the researchers found evidence of abundant and active C5aR1, which fuels glucosylceramide accumulation through its control of an enzyme that produces the fatty molecule. According to the authors, C5aR1 activation is what tips the balance between glucosylceramide formation and its degradation.
The researchers also found similar evidence of C5aR1 and related pro-inflammatory molecules in cells from the donated blood samples of Gaucher patients.
Experimental treatment
Based on evidence of C5aR1's involvement in the Gaucher disease process, the researchers decided to test targeting the molecule pharmacologically in laboratory mouse models. Taking advantage of a C5aR antagonist (C5aRA) developed by Köhl (patent owned by Cincinnati Children's), the scientists injected C5aRA into the peritoneal cavities of mice.
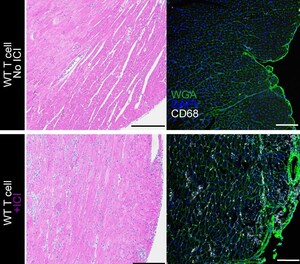
The infiltration of pro-inflammatory immune cells (macrophages) was substantially reduced in the lungs, livers and spleens of mice, and glucosylceramide accumulation was almost completely abolished, as was overall disease burden, the authors report.
Next steps
Because the current project was conducted in mouse models and human blood cells, Pandey and his colleagues stress that additional study is needed before determining whether targeting C5aR1 would be effective and safe enough to test in human patients.
Pandey said researchers will continue testing the C5aRA molecule used in the mouse study (which is effective in targeting human and mouse C5aR). They also will test a commercially available anti-C5 monoclonal antibody called eculizumab, which is produced by Alexion Pharmaceuticals (which helped fund the current study). This will allow the researchers to test these compounds as a novel adjunctive therapeutic approach for human patients with Gaucher, and as a possible therapy for other lysosomal storage diseases.
Funding support for the study came from Division of Human Genetics at Cincinnati Children's, the German Research Foundation (EXC 306/2, CL XII, IRTG 1911) and the Alexion Rare Disease Innovation Fund (31-91910-584000).
SOURCE Cincinnati Children's Hospital Medical Center






Share this article