TAMPA, Fla., June 1, 2022 /PRNewswire/ -- The Norman Parathyroid Center recognizes World Hypoparathyroidism Day, June 1, by highlighting its number one cause – surgeon inexperience. In fact, the incidence of this life-changing surgical complication can be more than 1000 times higher when the operation is performed by an inexperienced surgeon. But the use of human amniotic membrane provides great hope for the future.
Hypoparathyroidism is the combination of symptoms due to inadequate parathyroid hormone (PTH) production. Since the four parathyroid glands have complete control over the levels of calcium in the blood and bones, inadequate parathyroid gland function causes the blood calcium levels to decrease dramatically. If untreated with large doses of calcium, the patient can be expected to die within a week because of the failure of all muscles to contract and a complete failure of the musculature and nervous systems.
Hypoparathyroidism is a very rare condition in the general population where it can occur in mild to moderate forms due to genetic problems. However, hypoparathyroidism it is quite common following surgery for thyroid nodules and thyroid cancer due to the surgeon injuring or accidentally removing the parathyroid glands during the thyroid operation. It is estimated that more than 50% of patients undergoing thyroid surgery will have lack of parathyroid function for at least a few weeks, and as many as 5-6% will have hypoparathyroidism for the rest of their life.
On World Hypoparathyroidism Day, it is important to understand that more than 95% of patients with hypoparathyroidism have this problem as a complication from thyroid or parathyroid surgery. This is one of the most debilitating complications of any type of surgery performed on any area of the body because the lack of blood calcium affects the entire nervous system and every muscle of the body. And this complication is almost completely avoidable.
Hypoparathyroidism: A Life Altering Complication of Thyroid Surgery
Symptoms of hypoparathyroidism are lifelong and can be quite severe, including weak bones that break easily, kidney stones, excessive urination, stomach pain, weakness, fatigue, depression, anxiety, memory loss, bone and joint pain, nausea and more.
This condition makes people feel poorly often enough that nearly 25% of those suffering say they cannot work and have become unemployed because of this complication. Of those still working, 72% said they had to change jobs because of concentration abilities or other issues related to symptoms. 65% of patients say they miss 2 weeks or more of work per year more than they ever did before. These patients typically require doctor visits every 2-3 months for the rest of their lives, and many require visits to the emergency room every few months for additional calcium given intravenously.
Additionally, patients who had all of their parathyroid glands removed or destroyed during surgery will require high doses of calcium and Vitamin D every day for the rest of their lives. Less than 10% of all patients with hypoparathyroidism say their disease is managed well enough that they never have to go to the emergency room to receive IV calcium. Almost half of patients make one ER visit per year, while 25% make 3 or more ER visits per year. One third of patients with hypoparathyroidism are now required to see an endocrinologist every 1-2 months.
Hypoparathyroidism Study: Surgeon Experience Directly Related to Hypoparathyroidism
The Norman Parathyroid Center recently published the largest study of hypoparathyroid patients in the world. Data was collected from more than 200 patients suffering from hypoparathyroidism as a result of surgery on their thyroid or parathyroid glands. Almost every patient in this study was operated on by a surgeon who performs one or less parathyroid operations per month.
In this study of 215 patients with surgeon-induced hypoparathyroidism, the average age was 42 years and 90% were female. 80% were operated on for thyroid disease while 20% were operated on for parathyroid disease.
The Norman Parathyroid Center identified the surgeon responsible for each patient's complication and contacted their offices to establish the number of parathyroid or thyroid operations performed by that surgeon in the past two years. Every patient who developed hypoparathyroidism had a surgeon that performed thyroid/parathyroid surgery less than twice per week. 95% of the surgeons who caused this terrible complication performed less than one thyroid/parathyroid operation per week. 85% of the surgeons performed this operation less than once every two weeks. There were no patients with hypoparathyroidism in this study that had a surgeon who performed more than 150 of these operations per year.
Surgeons that performed between zero and five thyroid/parathyroid operations per year had a 9% chance of making their patient hypoparathyroid for life. The chance of this happening decreased to 5% when the surgeon performed 25 of these operations per year. It was not until the surgeon performed 150 or more thyroid/parathyroid operations annually that the rate of hypoparathyroidism decreased to the "acceptable" rate of 1% or less.
Sadly, over half of the patients who were made permanently hypoparathyroid by their surgeon never asked their surgeon about their experience in performing this operation. This group reported that it simply never occurred to them to ask, and that they further had no idea their surgeon did not do this operation often. 60% of patients said that the possibility of hypoparathyroid was never discussed with them prior to their operation.
Do Your Research – The Risk of Hypoparathyroidism is in Your Hands
World Hypoparathyroidism Day reminds us that the key to reducing the incidence of hypoparathyroidism lies in the hands of the patients. Patients must be educated about hypoparathyroidism as a life-changing complication PRIOR to undergoing surgery on their thyroid or parathyroid glands. Going to the "local surgeon" that your doctor sent you to is often not the best choice. Patients must check on the qualifications and experience of their surgeons if they expect the lowest possible complication rates.
"My wife has been struggling with hypoparathyroidism for years," says Bill from Atlanta, GA. "She had thyroid surgery for cancer and her parathyroid glands were destroyed. This has made her life miserable. She feels terrible all the time, has to take up to a dozen calcium pills per day, and has to go to the emergency room every 3-5 months to get additional calcium in an IV."
"Every week, I get multiple notes from patients who now have hypoparathyroidism as a consequence of their surgery," said Dr. Jim Norman, Founder and CEO of the Norman Parathyroid Center. "It's heartbreaking. They are suffering with horrible, debilitating symptoms and there is no way to fix it. It all could have been avoided by choosing a more experienced surgeon. My goal is to reach patients before they undergo thyroid or parathyroid surgery and educate them so that they can better advocate for themselves. There is no reason anyone should be suffering from surgeon-induced hypoparathyroidism."
New Methods Give Hope for Decreasing Hypoparathyroidism Following Thyroid Surgery
The expert thyroid surgeons at the Clayman Thyroid Center at the Hospital for Endocrine Surgery have been using human amniotic membrane to cover all parathyroid glands following thyroid surgery for the past 17 months. "The amniotic membrane contains growth factors and stem cells which promote tissue growth and viability," states Dr. Clayman. "Since we began using amniotic membrane, our incidence of temporary hypoparathyroidism has decreased from 18% to 3% and it only lasts a week or two instead of a month or two. This is a huge advantage for our patients, and we now we use it in all our thyroid operations."
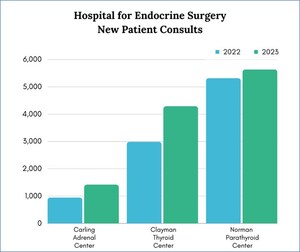
For over 20 years, the Norman Parathyroid Center's surgeons have been the highest-volume parathyroid surgeons in the world, performing nearly 3,800 parathyroid operations annually. Along with the surgeons of the Clayman Thyroid Center and the Carling Adrenal Center, they have recently moved into the new Hospital for Endocrine Surgery where the use of amniotic membrane on all exposed parathyroid glands following thyroid surgery has become standard of care, as well as during parathyroid surgery on any glands that have questionable viability. Aside from surgeon experience, the use of amniotic membrane appears to be the only means to decrease the incidence of this terrible disease.
About the Norman Parathyroid Center
Located in Tampa, Florida, the Norman Parathyroid Center is the leading parathyroid gland tumor treatment center in the world, performing nearly 3,800 parathyroid operations annually. Well known for cure rates over 99% via an operation that typically lasts about 20 minutes, the Norman Parathyroid Center's success centers on a teamwork approach by the most experienced parathyroid surgeons in the world.
www.parathyroid.com | (813) 972-0000
About the Clayman Thyroid Center
Founded by one of the nation's best-known thyroid surgeons, the Clayman Thyroid Center is the highest volume thyroid cancer referral center in the United States. The Center boasts the most experienced thyroid surgeons in the US who provide personalized care allowing the greatest opportunity for cancer cure, wellness, and cosmetic and functional outcomes via all types of thyroid surgery from minimal incision to scarless thyroid surgery to advanced cancer care.
www.thyroidcancer.com | (813) 940-3130
Contact:
Julie Canan, Director of Marketing
(941) 468 3002 – [email protected]
SOURCE Norman Parathyroid Center

WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
Newsrooms &
Influencers
Digital Media
Outlets
Journalists
Opted In




Share this article