Survey commissioned by Roche shows that HPV infection, which causes 99% of all cervical cancer cases, remains largely misunderstood by the general public
- Survey findings from over 8,700 people in 12 countries show that half of those polled have inadequate understanding of HPV, with nearly one-third being unsure or unaware of it altogether.1
- Findings also show that significant barriers continue to exist that are preventing women from seeking screening.1
- However, more than 70% of the respondents indicated they would be interested in the option of collecting their own sample for screening if available.
TUCSON, Ariz., Oct. 8, 2024 /PRNewswire/ -- GWI research commissioned by Roche (SIX: RO, ROG; OTCQX: RHHBY) and carried out across 12 countries in Latin America and Europe has revealed that half of those polled have either limited or no awareness of the important role human papillomavirus (HPV) plays in cervical cancer.1
HPV is a common virus transmitted through sexual contact and is the primary cause of cervical cancer, responsible for over 99% of cases.2 Every year, more than 600,000 women worldwide are diagnosed with cervical cancer and over 340,000 die, with nine in every ten of these women living in low-resource countries.3 However, 93% of cervical cancers could be prevented entirely through appropriate screening and HPV vaccination.4
The research also demonstrated that with screening rates varying between regions, significant barriers continue to exist that are preventing women from seeking testing.1 Respondents in all countries, including both developed and developing nations, reported that concerns about the testing procedure being painful were common (up to 63% in some countries), as well as a sense of discomfort about discussing their sexual history or sexuality with a healthcare provider (up to 57% in some countries).1
"Thousands of women are needlessly dying from cervical cancer every year. This survey highlights some of the most important barriers to screening, as well as the opportunities we have to prevent disease and improve women's health," said Joanna Sickler, Vice-President, Health Policy and External Affairs at Roche Diagnostics. "With many women reporting being open to new screening tools like self collection, it has never been more important that communities, health systems, governments and innovators come together to seize this opportunity, and provide the early detection and treatment needed to avoid so many preventable deaths."
The WHO is focused on accelerating the elimination of cervical cancer globally,2 with its latest guidelines recommending HPV DNA testing as primary screening for all women.5 Its strategy seeks to ensure that by 2030, 90% of girls are fully vaccinated against HPV by age 15. It also aims for 70% of women to have been screened using a high-performance test by age 35, and again by age 45, with 90% of those eligible linked to treatment. This, along with vaccination against HPV, could prevent more than 62 million deaths in the next 100 years.2
More than 50%of new cervical cancers occur in women who have never been screened, or have not been screened in the previous five years of their lives.6 Many factors can contribute to individuals not participating in cervical cancer screening programs, such as access to healthcare, social and economic barriers, history of traumatic experience, cultural concerns and embarrassment.
The many barriers preventing women from seeking HPV screening could explain the widespread interest in self-testing revealed by the survey. In European countries, where testing is more routinely available, 57% of women were interested in the opportunity to collect their own samples for testing. This figure rose to 77% in Latin American countries, where routine screening is less readily available because of a lack of infrastructure and available appointment means.
This discrepancy was also reflected in healthcare professional-reported results, which showed 72% of healthcare professionals and government workers in Latin American countries agree their country needs a self-collection programme, compared to 48% in Europe.
Susana Wong, Patient Advocate and Director of Lazo Rosado, Perú, is working to expand access to HPV testing in her country. She notes: "We know very well how to prevent and treat cervical cancer. Now, with HPV molecular tests and vaccination, there really is hope to eliminate this disease. This test gives you the opportunity to live and to live well with your family. It can help women to empower themselves as to their health."
Men demonstrated even lower levels of awareness compared to women, particularly in Europe. While 55% to 76% of men in Latin America reported some understanding of HPV, only 35% to 51% of men in Europe had any understanding of HPV at all. The lower awareness among men highlights the need for educational initiatives to include men, given their potential role in the transmission and prevention of HPV.
"This survey highlights both the challenges ahead and the significant opportunities we have to advance HPV prevention," Sickler said. "By enhancing public education about HPV risks and reimagining how we deliver care, we can drive higher screening rates and make meaningful progress in combating cervical cancer."
Fighting cervical cancer
Screening for HPV can help identify women who are at risk of developing cervical cancer, so that the disease can be treated early before invasive cancer has a chance to develop. In poorer countries, women are often diagnosed with cervical cancer at a more advanced stage, where the opportunity for a cure is low.
In September 2024, Roche officially joined the Global HPV Consortium. This presents an opportunity to collaborate globally, aligning our efforts with other organisations to advance cervical cancer prevention efforts and raise the prominence of early screening and timely detection using high-performance HPV-DNA tests.
Roche already partners with health systems and governments in more than 55 countries to support their cervical cancer screening programs with the cobas® HPV test. As a result of these collaborations, more women have been accessing HPV molecular testing. For example, since 2021, when Roche and the Perúvian Ministry of Health started working together, along with other government organisations and patient advocates, more than 300,000 unscreened or underscreened women, some in remote areas of the Amazon rainforest, have been tested for HPV using Roche's self-collection solution as the primary strategy to expand access.
The cobas® HPV test is also part of the Roche Global Access Program, which aims to improve access to cost-effective resources, implement scale-up programs, and contribute to the elimination of diseases in the regions with the greatest need.
About the Roche HPV Health Understanding Survey Conducted in Q1 2024, the HPV Health Understanding Survey was carried out by GWI on behalf of Roche. Surveying 8,703 men and women across 12 countries, it was designed to assess the general population's awareness of HPV and its role in the development of cervical cancer, as well as access to cervical health screening and barriers to care. It also measured perceptions among 2,585 healthcare professionals (HCPs) and government professionals of HPV testing availability in their own market.
Survey participants:
General population: n 8,704 Men and women aged 23-55 |
HCPs & government workers: n 2,585 |
Argentina: 505 |
Brazil: 241 |
Brazil: 542 |
Colombia: 300 |
Chile: 501 |
Ecuador: 100 |
Colombia: 505 |
France: 301 |
Ecuador 500 |
Germany: 300 |
France: 502 |
Italy: 301 |
Germany: 500 |
Mexico: 290 |
Italy: 507 |
Peru: 150 |
Mexico: 510 |
Spain: 301 |
Peru: 541 |
UK: 301 |
Spain: 501 |
|
UK: 504 |
About the Global Access Program
In 2014, Roche first launched its Global Access Program to support the UNAIDS 2020 targets to address the HIV/AIDS epidemic. Since then, the program has expanded to include solutions for other high-burden diseases such as Tuberculosis, Hepatitis B and C, and cervical cancer. Most recently, in response to the COVID-19 pandemic, the SARS-CoV-2 test was included into the program.
The continual expansion of test offerings highlights Roche's commitment to eliminating cervical cancer and other high-burden infectious diseases for patients living in resource-constrained settings with limited access.
Any laboratory that implements a Roche instrument system gains the ability to scale up testing across multiple disease areas, thus improving cost and resource efficiency. An integrated approach supports national programs focused on increasing access to diagnostic testing, to help manage or reduce the impact of preventable disease for patients.
About the Roche Diagnostics Cervical Cancer Portfolio
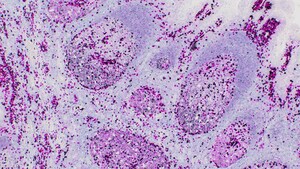
HPV is the known cause of virtually all cervical cancers.7 Roche Diagnostics' cervical cancer portfolio includes the cobas HPV test, used for primary screening and co-testing. While the Pap smear can potentially detect abnormalities in the cervix, cobas HPV detects 14 types of high-risk HPV genotypes that put patients at higher risk of developing cervical cancer. It includes results for HPV 16, HPV 18 and 12 other high-risk pooled genotypes.
The HPV self-collection solution is approved for use with Roche's cobas HPV test. The cobas HPV test runs on the cobas 4800 and the fully automated cobas 5800/6800/8800 Systems, which offers the fastest time to results, providing up to 96 results in about three hours, and 384 results for the cobas 6800 System and 1,056 results for the cobas 8800 System in an eight hour shift. The portfolio also includes CINtec PLUS Cytology, the only FDA-approved dual-stain product and CINtec® Histology, the only FDA-cleared p16 biomarker technology that can help pathologists confirm the presence of pre-cancerous cervical lesions.
The IMPACT trial design, used to validate the clinical benefits of the Roche cervical cancer portfolio, had representation from diverse patient segments, including 21 percent Black, 24 percent Hispanic-Latino and 0.3 percent American Indian or Alaskan Native participants8 . This diversity was critical to accurately assess the performance of dual stain in patient populations with higher incident rates of HPV. Learn more now: http://diagnostics.roche.com.
About Roche
Founded in 1896 in Basel, Switzerland, as one of the first industrial manufacturers of branded medicines, Roche has grown into the world's largest biotechnology company and the global leader in in-vitro diagnostics. The company pursues scientific excellence to discover and develop medicines and diagnostics for improving and saving the lives of people around the world. We are a pioneer in personalised healthcare and want to further transform how healthcare is delivered to have an even greater impact. To provide the best care for each person we partner with many stakeholders and combine our strengths in Diagnostics and Pharma with data insights from the clinical practice.
In recognising our endeavour to pursue a long-term perspective in all we do, Roche has been named one of the most sustainable companies in the pharmaceuticals industry by the Dow Jones Sustainability Indices for the thirteenth consecutive year. This distinction also reflects our efforts to improve access to healthcare together with local partners in every country we work.
Genentech, in the United States, is a wholly owned member of the Roche Group. Roche is the majority shareholder in Chugai Pharmaceutical, Japan.
For more information, please visit www.roche.com
All trademarks used or mentioned in this release are protected by law.
References
[1] GWI/Roche HPV Health Understanding Study 2024. Available at: https://www.roche.com/stories/survey-hpv-cervical-cancer
[2] Centers for Disease Control, Cancers caused by HPV https://www.cdc.gov/hpv/parents/cancer.html#:~:text=Cervical%20cancer%20and%20HPV,be%20prevented%20by%20HPV%20vaccination.
[3] World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. Article [Internet; updated 2020 November 17; cited 2023 Jan 3] Available from: https://www.who.int/publications/i/item/9789240014107
[4] World Health Organisation. Cervical Cancer Factsheet https://www.who.int/health-topics/cervical-cancer#tab=tab_1
[5] World Health Organization. 2020. Global strategy to accelerate the elimination of cervical cancer as a public health problem. Available at https://www.who.int/publications/i/item/9789240014107. Accessed 16 May 2023.
[6] Subramaniam A, Fauci JM, Schneider KE, Whitworth JM, Erickson BK, Kim K, Huh, WK. Invasive cervical cancer and screening: what are the rates of unscreened and underscreened women in the modern era? J Low Genit Tract Dis. 2011 Apr;15(2): 110-3. doi:10.1097/LGT.0b013e3181f515a2. PMID: 21263352; PMCID: PMC4465558. Accessed on 12 July 2024.
[7] National Cancer Institute. HPV and Cancer. Fact sheet [Internet; cited 2024 June 4] https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-and-cancer#:~:text=Sexually%20transmitted%20HPV%20types%20fall,for%20most%20HPV%2Drelated%20cancers
[8] Safaeian M, Wright TC Jr, Stoler MH, Ranger-Moore J, Rehm S, Aslam S, Fang Q, Volkir P, Ridder R. The IMproving Primary Screening And Colposcopy Triage trial: human papillomavirus, cervical cytology, and histopathologic results from the baseline and 1-year follow-up phase. Am J Obstet Gynecol. 2021 Sep;225(3):278.e1-278.e16. doi: 10.1016/j.ajog.2021.03.047. Epub 2021 Apr 20. PMID: 33852886
Roche Media Relations
Jo Lynn Garing
+1-317-363-7286
[email protected]
Amberly Peterson
+1-317-478-2210
[email protected]
Kathryn Ager
+44 07745 115046
[email protected]
SOURCE Roche

WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
Newsrooms &
Influencers
Digital Media
Outlets
Journalists
Opted In





Share this article