
CINCINNATI, Feb. 12, 2018 /PRNewswire-USNewswire/ -- Genomic profiling of mostly untreatable and deadly nerve sheath tumors led scientists to test a possible therapeutic strategy that inhibited tumor growth in lab tests on human tumor cells and mouse models, according to research in the journal Cancer Cell.
When the international team of researchers analyzed complete screens of genes and genetic material in malignant peripheral nerve sheath tumors (MPNSTs), it revealed previously unknown genetic information about the disease.
"This uncovered potential therapeutic targets we did not expect for these untreatable tumors, but our findings also need further study before knowing whether they will be relevant to patient treatment in the clinic," said Q. Richard Lu, PhD, lead author and scientific director of the Brain Tumor Center at the Cincinnati Children's Cancer and Blood Diseases Institute.
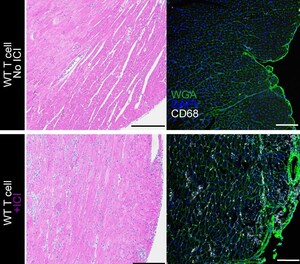
Researchers show a gene called Lats1/2 suppresses cancer, and losing the gene's expression reprograms cells so they rapidly expand and become cancerous. Loss of Lats1/2 also causes other genes in the HIPPO signaling pathway (which controls tissue growth) to become hyperactive. These hyperactive genes and their associated proteins (TAZ and YAP) then work with the protein TEAD1 to activate molecular cancer programs that form MPNSTs.
When researchers disrupted overactive TAZ-YAP in mice bred to lack Lats1/2, they also blocked signaling from PDGF (platelet-derived growth factor receptor), which supports tissue growth. These steps reduced the size and number of MPNSTs in the mice. They also inhibited the growth of human MPNST cells in laboratory cultures.
In their future work, Lu and his colleagues want to identify small-molecule agents that will inhibit TAZ-YAP and the downstream cancer programs they activate, he said. The researchers also need to identify druggable locations on the surface of MPNST cells or HIPPO signaling cascade inside cells. This would allow small molecular inhibitors to attach to and attack the tumor cells.
Like A Car Without Brakes
MPNST's develop in what are called Schwann cells. These cells form the myelin sheath. The myelin sheath functions as a protective insulation around peripheral nerves, which connect the brain and spinal cord to extremities and organs and promote transmission of nerve impulses.
About half of MPNSTs are linked to mutation of the NF1 gene, which causes a condition called Neurofibromatosis 1, researchers say. The other half of MPNSTs have no known genetic origins, and a small proportion of cases can be caused by radiotherapy given to people for cancer treatment, according to the authors.
The NF1 gene normally helps control a balanced rate of cell growth. When it mutates, it can cause brown spots on a person or benign tumors along peripheral nerves. In some cases, NF1 mutation can lead to cases of runaway cell growth, creating very large and sometimes medically problematic plexiform tumors which can turn into MPNSTs.
MPNSTs are biologically aggressive tumors and resistant to treatments like chemo and radiation therapy. They're also known for high relapse rates and poor prognosis, often leading to death.
More About the Study
The study's first author is Lai Man Natalie Wu, PhD, a research fellow in Lu's laboratory. The research also is a collaboration between multiple scientists at Cincinnati Children's and University Hospital in Dusseldorf, Germany, the German Cancer Consortium and German Cancer Research Center in Heidelberg, the Washington University School of Medicine in St. Louis, the MD Anderson Cancer Center in Houston, the University of Texas Southwestern Medical Center in Dallas, the Harvard Medical School in Boston.
Funding support for the research came in part from grants by the U.S. National Institutes of Health (R37NS096359, R01NS075243, R01 NS28840) and the Children's Tumor Foundation Young Investigator Award.
SOURCE Cincinnati Children's Hospital Medical Center





Share this article