Persistent Demand for Mental Healthcare via Telehealth during COVID-19 Pandemic, according to New FAIR Health Study
Over Two Years of Data Detail Telehealth's Evolution throughout the Pandemic
NEW YORK, June 14, 2022 /PRNewswire/ -- Since the onset of the COVID-19 pandemic, telehealth has undergone notable growth. It has been used for a wide array of health conditions and services that were overwhelmingly rendered in an office setting prior to COVID-19's emergence; these include mental health conditions, which have remained the most common telehealth diagnosis nationally throughout the pandemic. These and other findings on the changing nature of telehealth can be found in FAIR Health's new data brief released today, The Evolution of Telehealth during the COVID-19 Pandemic: A Multiyear Retrospective of FAIR Health's Monthly Telehealth Regional Tracker.
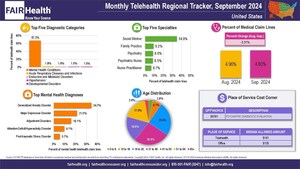
The newly released study provides a window into telehealth's changing contours using over two years of private healthcare claims data from FAIR Health's Monthly Telehealth Regional Tracker, a free, online tool that has tracked month-to-month changes in telehealth since the spring of 2020. Focusing on the period from January 2020 to March 2022, the brief reports on monthly changes in telehealth's utilization, top diagnoses and top procedure codes—in addition to other descriptive aspects of this venue of care—at national and regional (Midwest, Northeast, South, West) levels. Supported by infographics with vivid data visualizations, the brief also shows how the Monthly Telehealth Regional Tracker itself has evolved to meet the needs of healthcare stakeholders.
Among the key findings:
- From March 2019 to March 2020, the percentage of national telehealth claim lines when compared to all medical services increased 4,347 percent.1 The increase was even greater from April 2019 to April 2020 (8,336 percent).
- The top five telehealth diagnoses nationally in spring 2020 indicated that telehealth was being used for conditions that had not been among the top five the year before, including hypertension, joint/soft tissue diseases and issues, and developmental disorders.
- In November 2020, COVID-19 appeared for the first time on one of the regional lists of top five telehealth diagnoses, ranking fourth in the Midwest; in December 2020, COVID-19 emerged as a top telehealth diagnosis nationally and in every region.
- For 6 of the 12 months of 2021, telehealth utilization fell from the level of utilization in the prior month. Nevertheless, it remained much higher than before the pandemic. In December 2021, telehealth claim lines accounted for 4.9 percent of medical claim lines nationally, compared to 0.2 percent in December 2019.
- Many changes in telehealth utilization were likely related to the course of the pandemic. For example, in spring and summer 2021, telehealth claim lines dropped as vaccination levels increased. In fall and winter 2021, however, telehealth utilization rose again as the Delta and Omicron variants led to increased COVID-19 cases.
- Mental health conditions have been the most common telehealth diagnosis nationally throughout the pandemic. Consistent with that finding, in January 2022, social worker was the provider specialty rendering the most telehealth services (most commonly, psychotherapy) nationally and in every region but the West. In every region, as in the nation as a whole, three of the top five provider specialties were related to mental health: social worker, psychiatrist and psychologist.
- In January 2022, CPT®2 90837, one hour of psychotherapy, ranked highest among telehealth procedure codes nationally and in every region.
FAIR Health President Robin Gelburd stated: "In the wake of the COVID-19 pandemic, telehealth has become a material component of the nation's healthcare system. We hope that this brief provides actionable and relevant insights to healthcare stakeholders—including policy makers, researchers, payors, providers and consumers—seeking to better understand telehealth as it continues to evolve."
On Wednesday, June 22, from 2 to 3 pm ET, Ms. Gelburd will host a webinar entitled "Telehealth Utilization Before and During the COVID-19 Pandemic: A Two-Year Retrospective," which will provide insights on telehealth's evolution since winter 2020 using FAIR Health's comprehensive collection of telehealth data. Click here to register for the free, one-hour webinar.
For the new brief, click here.
Follow us on Twitter @FAIRHealth
FAIR Health is a national, independent nonprofit organization that qualifies as a public charity under section 501(c)(3) of the federal tax code. It is dedicated to bringing transparency to healthcare costs and health insurance information through data products, consumer resources and health systems research support. FAIR Health possesses the nation's largest collection of private healthcare claims data, which includes over 36 billion claim records and is growing at a rate of over 2 billion claim records a year. FAIR Health licenses its privately billed data and data products—including benchmark modules, data visualizations, custom analytics and market indices—to commercial insurers and self-insurers, employers, providers, hospitals and healthcare systems, government agencies, researchers and others. Certified by the Centers for Medicare & Medicaid Services (CMS) as a national Qualified Entity, FAIR Health also receives data representing the experience of all individuals enrolled in traditional Medicare Parts A, B and D; FAIR Health includes among the private claims data in its database, data on Medicare Advantage enrollees. FAIR Health can produce insightful analytic reports and data products based on combined Medicare and commercial claims data for government, providers, payors and other authorized users. FAIR Health's systems for processing and storing protected health information have earned HITRUST CSF certification and achieved AICPA SOC 2 compliance by meeting the rigorous data security requirements of these standards. As a testament to the reliability and objectivity of FAIR Health data, the data have been incorporated in statutes and regulations around the country and designated as the official, neutral data source for a variety of state health programs, including workers' compensation and personal injury protection (PIP) programs. FAIR Health data serve as an official reference point in support of certain state balance billing laws that protect consumers against bills for surprise out-of-network and emergency services. FAIR Health also uses its database to power a free consumer website available in English and Spanish, which enables consumers to estimate and plan for their healthcare expenditures and offers a rich educational platform on health insurance. An English/Spanish mobile app offers the same educational platform in a concise format and links to the cost estimation tools. The website has been honored by the White House Summit on Smart Disclosure, the Agency for Healthcare Research and Quality (AHRQ), URAC, the eHealthcare Leadership Awards, appPicker, Employee Benefit News and Kiplinger's Personal Finance. FAIR Health also is named a top resource for patients in Dr. Marty Makary's book The Price We Pay: What Broke American Health Care—and How to Fix It and Dr. Elisabeth Rosenthal's book An American Sickness: How Healthcare Became Big Business and How You Can Take It Back. For more information on FAIR Health, visit fairhealth.org.
Contact:
Rachel Kent
Senior Director of Marketing
FAIR Health
646-396-0795
[email protected]
1 A claim line is an individual service or procedure listed on an insurance claim.
2 CPT © 2021 American Medical Association (AMA). All rights reserved.
SOURCE FAIR Health

WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
Newsrooms &
Influencers
Digital Media
Outlets
Journalists
Opted In




Share this article