
CINCINNATI, March 9, 2015 /PRNewswire-USNewswire/ -- Preclinical research demonstrates for the first time that refocusing an expectant mother's immune cells to prevent them from attacking the fetus may be a therapeutic strategy for preventing pregnancy complications like stillbirth or prematurity.
Scientists at Cincinnati Children's Hospital Medical Center report their findings March 9 in The Journal of Clinical Investigation. They suggest restricting the pregnant mother's immune cells from the placenta (the maternal-fetal interface) can protect against pregnancy complications during prenatal infection and those not caused by infection.
The study sheds new light on an entrenched public health challenge – premature birth and the related pregnancy complications of preeclampsia, spontaneous abortion and stillbirth. One of every 9 infants in the United States is born premature, or before 37 weeks of pregnancy, according to the U.S. Centers for Disease Control. There remains no effective therapy for these pregnancy complications, and babies born too early are highly vulnerable to death or long-term developmental abnormalities.
Although the causes of premature birth and most pregnancy complications are not completely known, maternal infection is consistently identified as an important contributor, according to senior study author Sing Sing Way, MD, PhD, a pediatrician in the Division of Infectious Diseases and the Cincinnati Children's Perinatal Institute.
"Pregnant women are especially susceptible to infection, so it might seem counter intuitive to prevent their immune cells from properly penetrating placental tissues," said Way. "However, we found that pregnancy complications largely stem from harmful maternal immune cells that recognize and attack the placenta and other immunologically foreign tissues derived from the fetus. Restricting the access of harmful immune cells to developmentally delicate fetal tissue represents a highly innovative therapeutic strategy."
Way said the immune system of a pregnant mother has a delicate balancing act – sustaining protection against infection while trying not to harm the baby from over-reactive immune responses. This means that any proposed therapy that modulates a pregnant mother's immune system must be very precise.
Along with first author and Cincinnati Children's researcher Vandana Chaturvedi, PhD, the team used mouse models of human pregnancy to evaluate pregnancy outcomes after infection and experimental manipulations of maternal immune components. The scientists used a bacterium commonly found in the environment and food supply, Listeria monocytogenes, to infect pregnant mice. In humans, Listeria causes severe invasive infection in the mother during pregnancy with often fatal consequences for the fetus.
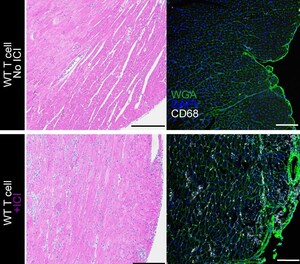
When researchers infected pregnant mice with Listeria, they found specialized subsets of first-responder immune cells (neutrophils and macrophages) that rapidly infiltrate the placenta. These inflammatory cells produce high levels of a chemoattractant protein, CXCL9. This paves the way for harmful T cells that specifically recognize and attack the fetus.
Way said this initial finding is significant because harmful immune components that recognize the fetus are normally restricted from the placenta. Cells in placental tissue are specifically programmed not to express chemokines or chemoattractant proteins like CXCL9, serving as a protective barrier for the fetus.
After pregnant mothers are infected by Listeria, the protective barrier is circumvented. This unleashes harmful T cells directly to the placenta and fetus. After infection in pregnant mice, it leads to fetal resorption and stillbirth.
The researchers then discovered that selectively neutralizing CXCL9 activity by blocking its receptor on T cells, CXCR3, kept harmful immune cells from infiltrating the placenta. This prevented stillbirth.
Way and colleagues experimentally blocked CXCR3 in a couple of ways. First, they used pregnant mice genetically deleted of the CXCR3 chemokine receptor, so it was not present during prenatal Listeria infection. In a second complementary approach, a protein or antibody with CXCR3 neutralizing properties was administered to pregnant mice.
Regardless of methodology, blocking CXCR3 effectively eliminated fetal resorption and restored healthy live offspring to Listeria infected mice. Blocking CXCR3 with a neutralizing antibody also prevented stillbirth despite delayed administration to pregnant mice already infected with Listeria.
Researchers also conducted tests to see if blocking CXCR3 would apply to pregnancy complications not caused by prenatal infection. The team used an approach where fetal injury was instead caused by depleting a protective immune-suppressive subset of maternal T cells called regulatory T cells. These cells naturally expand in women during healthy pregnancies, but not in pregnancies complicated by preeclampsia or spontaneous abortion. They found that CXCR3 blockade prevented fetal loss after the depletion of regulatory T cells.
Although researchers focused on animal pregnancy in the current study, the findings will likely extend to complications in human pregnancy, Way said. This is because humans and other mammals share susceptibility to Listeria monocytogenes prenatal infection.
Because the actual causes of pregnancy complications are unknown – and not identified in most pregnancies – therapeutically preventing harmful immune cells from entering the placenta targets a more common root of fetal injury, Way said. He added the strategy should have broader applicability for infectious and non-infectious causes of pregnancy complications.
Small molecule inhibitors that block CXCR3 and its related chemokines are currently being tested for the treatment of human autoimmune and inflammatory disorders. As the next step in their research, Way and his colleagues want to test these inhibitors in pregnancy models to see if they provide similar levels of protection from pregnancy complications.
"We hope the findings from this study will spark renewed interest across the biomedical community in establishing the underlying causes of pregnancy complications, and development of new therapeutic strategies for ensuring healthy pregnancy and healthy children," Way said.
Funding support for the study came from the National Institute of Allergy and Infectious Diseases (grants R01-AI087830, R01-AI100934, R21-AI112186), and an Investigator in the Pathogenesis of Infectious Disease award from the Burroughs Wellcome Fund.
About Cincinnati Children's:
Cincinnati Children's Hospital Medical Center ranks third in the nation among all Honor Roll hospitals in U.S. News and World Report's 2014 Best Children's Hospitals. It is also ranked in the top 10 for all 10 pediatric specialties. Cincinnati Children's, a non-profit organization, is one of the top three recipients of pediatric research grants from the National Institutes of Health, and a research and teaching affiliate of the University of Cincinnati College of Medicine. The medical center is internationally recognized for improving child health and transforming delivery of care through fully integrated, globally recognized research, education and innovation. Additional information can be found at www.cincinnatichildrens.org. Connect on the Cincinnati Children's blog, via Facebook and on Twitter.
Logo - http://photos.prnewswire.com/prnh/20110406/MM79025LOGO
SOURCE Cincinnati Children's Hospital Medical Center






Share this article