In April, Telehealth Utilization Increased Nationally and in South, but Decreased in Other Regions; Telehealth Utilization in South Increased by 7.2 Percent from March to April
Mental Health Conditions Rose as a Percentage of Telehealth Claim Lines Nationally and in Every Region, While Acute Respiratory Diseases and Infections Fell
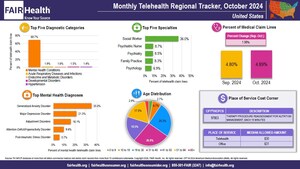
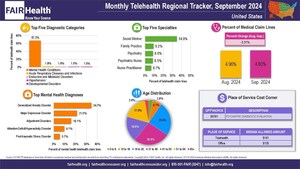
NEW YORK, July 15, 2024 /PRNewswire/ -- In April 2024, telehealth utilization increased nationally and in the South, but decreased in the three other US census regions (Midwest, Northeast and West), according to FAIR Health's Monthly Telehealth Regional Tracker. Nationally, telehealth claim lines rose from 4.73 percent of medical claim lines in March to 4.86 percent in April, an increase of 2.7 percent.1 In the South, the increase was 7.2 percent, from 3.48 percent of medical claim lines in March to 3.73 percent in April. In the Midwest, the telehealth share of medical claim lines fell 0.4 percent; in the Northeast, it fell 3.0 percent; and in the West, it fell 3.3 percent. The data represent the commercially insured population, excluding Medicare Fee-for-Service, Medicare Advantage and Medicaid.
Diagnostic Categories
Nationally and in every region, from March to April 2024, acute respiratory diseases and infections fell in percent of telehealth claim lines. In three regions, this diagnostic category also declined in the rankings of the top five telehealth diagnostic categories: from third to fifth position in the Midwest, from second to fifth position in the Northeast and from fourth to fifth position in the West.
During the same period, mental health conditions rose in percent of telehealth claim lines nationally and in every region. Mental health conditions remained the top-ranking diagnostic category nationally and in every region.
Nationally, the diagnostic categories in the third, fourth and fifth positions changed from March to April. In March, they were, respectively, encounter for examination, endocrine and metabolic disorders and developmental disorders; in April, they were, respectively, endocrine and metabolic disorders, developmental disorders and encounter for examination.
Mental Health Diagnoses
There was no change in the rankings of the top five mental health diagnoses from March to April 2024. Nationally and in every region, the top five mental health diagnoses in both months were: generalized anxiety disorder, major depressive disorder, adjustment disorders, attention-deficit/hyperactivity disorder and post-traumatic stress disorder. Together, generalized anxiety disorder and major depressive disorder accounted for more than 50 percent of mental health telehealth claim lines nationally and in every region in both months.
Specialties
From March to April 2024, at the national level, there were some changes in the rankings of the top five telehealth provider specialties. Family practice fell from second to fourth position, while psychiatry and psychiatric nurse rose from, respectively, third and fourth position to second and third position. The rankings of the top five telehealth provider specialties remained unchanged in every region.
Social worker remained in the first position nationally and in all regions.
Age
In April 2024, as in March, the age group 31 to 40 accounted for the largest share of telehealth claim lines nationally and in the South and West, while the age group 19 to 30 accounted for the largest share in the Midwest and Northeast. In both months, the age groups 19-30 and 31-40 each accounted for more than 20 percent of telehealth claim lines nationally and in every region.
Costs
Nationally and in every region but the West, the median allowed amount2 for CPT®3 99457 (management using the results of remote vital sign monitoring per calendar month, first 20 minutes) in April 2024 was higher when rendered via telehealth than in an office. The highest median values for both telehealth ($65) and office ($60) occurred in the Northeast. In both the South and Midwest, the median telehealth cost was $57 and the office cost was $51. In the West, the median telehealth cost was $53 and the office cost $54. Nationally, the median telehealth cost was $55 and the office cost $53.
About the Monthly Telehealth Regional Tracker
Launched in May 2020 as a free service, the Monthly Telehealth Regional Tracker uses FAIR Health data to track how telehealth is evolving from month to month. An interactive map of the four US census regions allows the user to view an infographic on telehealth in a specific month in the nation as a whole or in individual regions. Each year, the infographic introduces varied views into telehealth utilization. In this fifth iteration of the Monthly Telehealth Regional Tracker, each infographic shows month-to-month changes in volume of telehealth claim lines; that month's top five diagnostic categories, mental health diagnoses and specialties; age distribution; and the Place of Service Cost Corner, which compares median allowed amounts for a specific procedure provided via telehealth to the same procedure provided in an office.
FAIR Health President Robin Gelburd stated: "We are happy to share these continuing windows into telehealth utilization as this venue of care evolves. This is one of the many ways we pursue our healthcare transparency mission."
For the Monthly Telehealth Regional Tracker, click here.
Follow us on X @FAIRHealth
About FAIR Health
FAIR Health is a national, independent nonprofit organization that qualifies as a public charity under section 501(c)(3) of the federal tax code. It is dedicated to bringing transparency to healthcare costs and health insurance information through data products, consumer resources and health systems research support. FAIR Health possesses the nation's largest collection of commercial healthcare claims data, which includes over 47 billion claim records and is growing at a rate of over 3 billion claim records a year. FAIR Health licenses its commercial data and data products—including benchmark modules, data visualizations, custom analytics and market indices—to commercial insurers and self-insurers, employers, providers, hospitals and healthcare systems, government agencies, researchers and others. Certified by the Centers for Medicare & Medicaid Services (CMS) as a national Qualified Entity, FAIR Health also receives data representing the experience of all individuals enrolled in traditional Medicare Parts A, B and D, which accounts for a separate collection of over 48 billion claim records; FAIR Health includes among the commercial claims data in its database, data on Medicare Advantage enrollees. FAIR Health can produce insightful analytic reports and data products based on combined Medicare and commercial claims data for government, providers, payors and other authorized users. FAIR Health's systems for processing and storing protected health information have earned HITRUST CSF certification and achieved AICPA SOC 2 Type 2 compliance by meeting the rigorous data security requirements of these standards. As a testament to the reliability and objectivity of FAIR Health data, the data have been incorporated in statutes and regulations around the country and designated as the official, neutral data source for a variety of state health programs, including workers' compensation and personal injury protection (PIP) programs. FAIR Health data serve as an official reference point in support of certain state balance billing laws that protect consumers against bills for surprise out-of-network and emergency services. FAIR Health also uses its database to power a free consumer website available in English and Spanish, which enables consumers to estimate and plan for their healthcare expenditures and offers a rich educational platform on health insurance. An English/Spanish mobile app offers the same educational platform in a concise format and links to the cost estimation tools. The website has been honored by the White House Summit on Smart Disclosure, the Agency for Healthcare Research and Quality (AHRQ), URAC, the eHealthcare Leadership Awards, appPicker, Employee Benefit News and Kiplinger's Personal Finance. For more information on FAIR Health, visit fairhealth.org.
Contact:
Rachel Kent
Executive Director of Communications and Marketing
FAIR Health
646-396-0795
[email protected]
1 A claim line is an individual service or procedure listed on an insurance claim.
2 An allowed amount is the total fee paid to the provider under an insurance plan. It includes the amount that the health plan pays and the part the patient pays under the plan's in-network cost-sharing provisions (e.g., copay or coinsurance if the patient has met the deductible).
3 CPT © 2023 American Medical Association (AMA). All rights reserved.
SOURCE FAIR Health

WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
Newsrooms &
Influencers
Digital Media
Outlets
Journalists
Opted In




Share this article