European Commission Approves RINVOQ® (upadacitinib) as First JAK Inhibitor in the European Union for the Treatment of Both Adults and Adolescents with Moderate to Severe Atopic Dermatitis
- Approval supported by data from one of the largest registrational Phase 3 programs in atopic dermatitis evaluating RINVOQ (upadacitinib) monotherapy or with topical corticosteroids[1]
- RINVOQ met all primary and secondary endpoints, demonstrating rapid and significant improvement in skin clearance and itch reduction compared to placebo at week 16 and earlier time points (p<0.001)[1]
- Results at week 16 continued to be maintained through week 52[1]
- RINVOQ has a safety profile supported by clinical programs evaluating more than 10,500 patients* across approved indications, and on-market experience in rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis[2-9]
- Milestone marks the fourth EC-approved indication for RINVOQ[1]
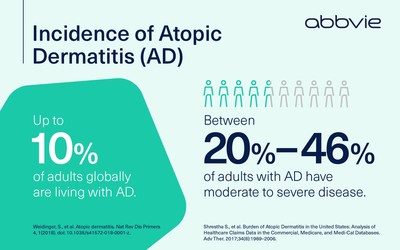
NORTH CHICAGO, Ill., Aug. 24, 2021 /PRNewswire/ -- AbbVie (NYSE: ABBV) today announced the European Commission (EC) approved RINVOQ® (upadacitinib), an oral, selective and reversible JAK inhibitor, for the treatment of moderate to severe atopic dermatitis in adults and adolescents 12 years and older who are candidates for systemic therapy.1 The recommended dose of RINVOQ for atopic dermatitis in adults is 15 mg or 30 mg once daily based on individual patient presentation, and 15 mg once daily for adolescents (12-17 years of age) and adults 65 years and older.1 RINVOQ can be used with or without topical corticosteroids (TCS).1
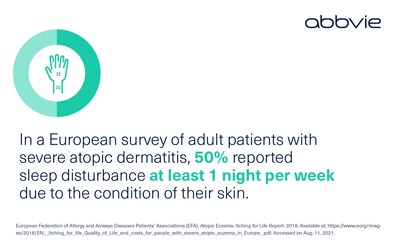
"This is a significant milestone for AbbVie in our pursuit to transform care in atopic dermatitis," said Michael Severino, M.D., vice chairman and president, AbbVie. "We are excited to provide an additional treatment option in Europe to help alleviate the burden of unrelenting itch and rash that many of these patients struggle with in daily life, despite available treatment options."
The EC approval is supported by data from one of the largest registrational Phase 3 programs in atopic dermatitis with more than 2,500 adults and adolescents with moderate to severe disease.1 These studies evaluated the efficacy and safety of RINVOQ monotherapy (Measure Up 1 [MU1] and Measure Up 2 [MU2]) and with topical corticosteroids (AD Up [AU]) compared to placebo.1 In all three studies, the co-primary endpoints were at least a 75 percent improvement in the Eczema Area and Severity Index (EASI 75) and validated Investigator's Global Assessment for Atopic Dermatitis (vIGA-AD) score of 0/1 (clear or almost clear) at week 16.1
"As a dermatologist researching and treating atopic dermatitis for more than 25 years, I've seen first-hand the debilitating impact this disease can have on a person's daily life," said Alan Irvine, M.D., D.Sc., professor of dermatology, Trinity College Dublin, Ireland, and RINVOQ clinical study investigator. "Clinicians need more tools to help them treat and manage this complex disease. The degree and early onset of skin clearance and itch relief in the RINVOQ Phase 3 clinical studies are very encouraging. The outcomes have the potential to advance treatment goals for patients with moderate to severe atopic dermatitis."
Highlights From the Global Phase 3 Atopic Dermatitis Clinical Trial Program1
Across the Phase 3 studies, all primary and secondary endpoints were met with 15 mg and 30 mg doses of RINVOQ compared to placebo. Highlights include:
- Significantly more patients achieved EASI 75 at week 16 in the RINVOQ 15 mg group (MU1: 70%; MU2: 60%; AU: 65%) and the RINVOQ 30 mg group (MU1: 80%; MU2: 73%; AU: 77%), compared to placebo (MU1: 16%; MU2: 13%; AU: 26%).
- Significantly more patients achieved vIGA-AD 0/1 at week 16 in the RINVOQ 15 mg group (MU1: 48%; MU2: 39%; 40: 31%) and the RINVOQ 30 mg group (MU1: 62%; MU2: 52%; AU: 59%) compared to placebo (MU1: 8%; MU2: 5%; AU: 11%).
- Significantly more patients achieved clinically meaningful itch reduction (improvement in Worst Pruritus NRS ≥4) in the RINVOQ 15 mg group (MU1: 52%; MU2: 42%; AU: 52%) and the RINVOQ 30 mg group (MU1: 60%; MU2: 60%; AU: 64%) compared to placebo (MU1: 12%; MU2: 9%; AU: 15%) at week 16.
- Clinically meaningful itch reduction (improvement in Worst Pruritus NRS ≥4) and skin clearance (EASI 75) were observed as early as week 1 and week 2, respectively, in patients treated with either dose of RINVOQ compared to those treated with placebo.
- Results at week 16 continued to be maintained through week 52 in patients treated with either dose of RINVOQ.
The most commonly reported adverse reactions (≥5% of patients) with RINVOQ 15 mg or 30 mg were upper respiratory tract infection (25.4%), acne (15.1%), herpes simplex (8.4%), headache (6.3%) and increased blood creatine phosphokinase (CPK; 5.5%).1 The most common serious adverse reactions were serious infections (<1.0%).1
The Marketing Authorization means that RINVOQ is approved in all member states of the European Union, as well as Iceland, Liechtenstein, Norway and Northern Ireland. RINVOQ is already approved for the treatment of moderate to severe atopic dermatitis in Russia, Saudi Arabia, United Arab Emirates, New Zealand and Chile, and is currently under review in the U.S. by the Food and Drug Administration (FDA).
*10,500 patients includes all patients across all arms (active treatment and placebo) in 8 Phase 3 trials in rheumatoid arthritis, 2 in psoriatic arthritis, 1 in ankylosing spondylitis and 5 in atopic dermatitis.2-9 This includes 344 adolescent patients (aged 12 to 17 years) in the Phase 3 Measure Up 1, Measure Up 2 and, AD Up studies in atopic dermatitis.1,2,5 Of the total number of patients included in these trials, 6,280 were randomized to receive RINVOQ at either dose.2-9
About RINVOQ® (upadacitinib)
Discovered and developed by AbbVie scientists, RINVOQ is a selective and reversible JAK inhibitor that is being studied in several immune-mediated inflammatory diseases.1,10-20 In human cellular assays, RINVOQ preferentially inhibits signaling by JAK1 or JAK1/3 with functional selectivity over cytokine receptors that signal via pairs of JAK2.1 RINVOQ 15 mg is also approved by the U.S. Food and Drug Administration (FDA) for adults with moderately to severely active rheumatoid arthritis, and by the European Commission for adults with moderate to severe active rheumatoid arthritis, adults with active psoriatic arthritis (PsA) and adults with active ankylosing spondylitis (AS). Phase 3 trials of RINVOQ in rheumatoid arthritis, atopic dermatitis, psoriatic arthritis, axial spondyloarthritis, Crohn's disease, ulcerative colitis, giant cell arteritis and Takayasu arteritis are ongoing.12-20
Important EU Indications and Safety Information about RINVOQ® (upadacitinib)1
Rheumatoid arthritis
RINVOQ is indicated for the treatment of moderate to severe active rheumatoid arthritis in adult patients who have responded inadequately to, or who are intolerant to one or more disease-modifying anti-rheumatic drugs (DMARDs). RINVOQ may be used as monotherapy or in combination with methotrexate.
Psoriatic arthritis
RINVOQ is indicated for the treatment of active psoriatic arthritis in adult patients who have responded inadequately to, or who are intolerant to one or more DMARDs. RINVOQ may be used as monotherapy or in combination with methotrexate.
Ankylosing spondylitis
RINVOQ is indicated for the treatment of active ankylosing spondylitis in adult patients who have responded inadequately to conventional therapy.
Atopic dermatitis
RINVOQ is indicated for the treatment of moderate to severe atopic dermatitis in adults and adolescents 12 years and older who are candidates for systemic therapy.
Contraindications
RINVOQ is contraindicated in patients hypersensitive to the active substance or to any of the excipients, in patients with active tuberculosis (TB) or active serious infections, in patients with severe hepatic impairment, and during pregnancy.
Special warnings and precautions for use
Immunosuppressive medicinal products
Use in combination with other potent immunosuppressants is not recommended.
Serious infections
Serious and sometimes fatal infections have been reported in patients receiving upadacitinib. The most frequent serious infections reported included pneumonia and cellulitis. Cases of bacterial meningitis have been reported. Among opportunistic infections, TB, multidermatomal herpes zoster, oral/esophageal candidiasis, and cryptococcosis have been reported with upadacitinib. As there is a higher incidence of infections in patients ≥65 years of age, caution should be used when treating this population.
Viral reactivation
Viral reactivation, including cases of herpes zoster, was reported in clinical studies. The risk of herpes zoster appears to be higher in Japanese patients treated with upadacitinib.
Vaccinations
The use of live, attenuated vaccines during or immediately prior to therapy is not recommended. It is recommended that patients be brought up to date with all immunizations, including prophylactic zoster vaccinations, prior to initiating upadacitinib, in agreement with current immunization guidelines.
Malignancy
The risk of malignancies, including lymphoma is increased in patients with rheumatoid arthritis (RA). Malignancies, including nonmelanoma skin cancer (NMSC), have been reported in patients treated with upadacitinib. Consider the risks and benefits of upadacitinib treatment prior to initiating therapy in patients with a known malignancy other than a successfully treated NMSC or when considering continuing upadacitinib therapy in patients who develop a malignancy.
Hematological abnormalities
Treatment should not be initiated, or should be temporarily interrupted, in patients with hematological abnormalities observed during routine patient management.
Cardiovascular risk
RA patients have an increased risk for cardiovascular disorders. Patients treated with upadacitinib should have risk factors (e.g., hypertension, hyperlipidemia) managed as part of usual standard of care.
Lipids
Upadacitinib treatment was associated with dose-dependent increases in lipid parameters, including total cholesterol, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol.
Hepatic transaminase elevations
Treatment with upadacitinib was associated with an increased incidence of liver enzyme elevation compared to placebo.
Venous thromboembolisms
Events of deep vein thrombosis (DVT) and pulmonary embolism (PE) have been reported in patients receiving JAK inhibitors, including upadacitinib. Upadacitinib should be used with caution in patients at high risk for DVT/PE.
Adverse reactions
The most commonly reported adverse reactions in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis clinical trials (≥2% of patients in at least one of the indications) with upadacitinib 15 mg were upper respiratory tract infections, blood creatine phosphokinase (CPK) increased, alanine transaminase increased, bronchitis, nausea, cough, aspartate transaminase increased, and hypercholesterolemia.
The most commonly reported adverse reactions in atopic dermatitis trials (≥2% of patients) with upadacitinib 15 mg or 30 mg were upper respiratory tract infection, acne, herpes simplex, headache, CPK increased, cough, folliculitis, abdominal pain, nausea, neutropenia, pyrexia, and influenza.
Ankylosing spondylitis:
Overall, the safety profile observed in patients with active ankylosing spondylitis treated with upadacitinib 15 mg was consistent with the safety profile observed in patients with RA.
Psoriatic arthritis:
Overall, the safety profile observed in patients with active psoriatic arthritis treated with upadacitinib 15 mg was consistent with the safety profile observed in patients with RA. A higher incidence of acne and bronchitis was observed in patients treated with upadacitinib 15 mg (1.3% and 3.9%, respectively) compared to placebo (0.3% and 2.7%, respectively). A higher rate of serious infections (2.6 events per 100 patient-years and 1.3 events per 100 patient-years, respectively) and hepatic transaminase elevations (ALT elevations Grade 3 and higher rates 1.4% and 0.4%, respectively) was observed in patients treated with upadacitinib in combination with MTX therapy compared to patients treated with monotherapy. There was a higher rate of serious infections in patients ≥65 years of age, although data are limited.
Atopic dermatitis:
Dose-dependent changes in ALT increased and/or AST increased (≥ 3 x ULN), lipid parameters, CPK values (> 5 x ULN), and neutropenia (ANC < 1 x 109 cells/L) associated with upadacitinib treatment were similar to what was observed in the rheumatologic disease clinical studies. Based on limited data in atopic dermatitis patients aged 65 years and older, there was a higher rate of overall adverse reactions with the upadacitinib 30 mg dose compared to the 15 mg dose. The safety profile for upadacitinib 15 mg in adolescents was similar to that in adults. The safety and efficacy of the 30 mg dose in adolescents are still being investigated.
This is not a complete summary of all safety information.
Please see the RINVOQ full SmPC for complete prescribing information at http://www.EMA.europa.eu.
Globally, prescribing information varies; refer to the individual country product label for complete information.
About AbbVie
AbbVie's mission is to discover and deliver innovative medicines that solve serious health issues today and address the medical challenges of tomorrow. We strive to have a remarkable impact on people's lives across several key therapeutic areas: immunology, oncology, neuroscience, eye care, virology, women's health and gastroenterology, in addition to products and services across its Allergan Aesthetics portfolio. For more information about AbbVie, please visit us at www.abbvie.com. Follow @abbvie on Twitter, Facebook, LinkedIn or Instagram.
Forward-Looking Statements
Some statements in this news release are, or may be considered, forward-looking statements for purposes of the Private Securities Litigation Reform Act of 1995. The words "believe," "expect," "anticipate," "project" and similar expressions, among others, generally identify forward-looking statements. AbbVie cautions that these forward-looking statements are subject to risks and uncertainties that may cause actual results to differ materially from those indicated in the forward-looking statements. Such risks and uncertainties include, but are not limited to, failure to realize the expected benefits from AbbVie's acquisition of Allergan plc ("Allergan"), failure to promptly and effectively integrate Allergan's businesses, competition from other products, challenges to intellectual property, difficulties inherent in the research and development process, adverse litigation or government action, changes to laws and regulations applicable to our industry and the impact of public health outbreaks, epidemics or pandemics, such as COVID-19. Additional information about the economic, competitive, governmental, technological and other factors that may affect AbbVie's operations is set forth in Item 1A, "Risk Factors," of AbbVie's 2020 Annual Report on Form 10-K, which has been filed with the Securities and Exchange Commission, as updated by its subsequent Quarterly Reports on Form 10-Q. AbbVie undertakes no obligation to release publicly any revisions to forward-looking statements as a result of subsequent events or developments, except as required by law.
References:
- RINVOQ [Summary of Product Characteristics]. AbbVie Deutschland GmbH & Co. KG; August 2021. Available at: https://www.ema.europa.eu/en/documents/product-information/rinvoq-epar-product-information_en.pdf.
- Guttman-Yassky E., et al. Once-daily upadacitinib versus placebo in adolescents and adults with moderate-to-severe atopic dermatitis (Measure Up 1 and Measure Up 2): results from two replicate double-blind, randomised controlled phase 3 trials. Lancet. 2021; 397(10290): 2151-2168. doi:10.1016/S0140-6736(21)00588-2.
- Blauvelt A., et al. Efficacy and Safety of Upadacitinib vs Dupilumab in Adults With Moderate-to-Severe Atopic Dermatitis: A Randomized Clinical Trial. JAMA Dermatol. Published online August 4, 2021. doi:10.1001/jamadermatol.2021.3023.
- EPAR: RINVOQ [European Public Assessment Report]. AbbVie Deutschland GmbH & Co. KG. June 2021. Available at: https://www.ema.europa.eu/en/medicines/human/EPAR/rinvoq.
- Reich K, Teixeira HD, Bruin-Weller, et al. Safety and efficacy of upadacitinib in combination with topical corticosteroids in adolescents and adults with moderate-to-severe atopic dermatitis (AD Up): results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2021; 397(10290): 2169-2181.
- Zeng, X., et al. SAT0160 Efficacy and Safety of Upadacitinib In Patients From China, Brazil, And South Korea With Rheumatoid Arthritis Who Have Had Inadequate Response To Conventional Synthetic Disease-Modifying Antirheumatic Drugs. Ann Rheum Dis. 2020. 79:1020-1021.
- Rubbert-Roth A., et al. Trial of Upadacitinib or Abatacept in Rheumatoid Arthritis. N Engl J Med. 2020;383(16):1511-1521. doi:10.1056/NEJMoa2008250.
- Kameda H., et al. Efficacy and safety of upadacitinib in Japanese patients with rheumatoid arthritis (SELECT-SUNRISE): a placebo-controlled phase llb/lll study. Rheumatology (Oxford). 2020;59(11):3303-3313. doi:10.1093/rheumatology/keaa084.
- A Study to Evaluate Safety of Upadacitinib in Combination With Topical Corticosteroids in Adolescent and Adult Participants With Moderate to Severe Atopic Dermatitis (Rising Up). ClinicalTrials.gov. 2020. Available at: https://clinicaltrials.gov/ct2/show/NCT03661138. Accessed on August 19, 2021.
- Cohen S., et al. Safety profile of upadacitinib in rheumatoid arthritis: integrated analysis from the SELECT phase III clinical programme. Ann Rheum Dis. 2020 Oct 28;80(3):304-11.
- Mease, P.J., et al. Upadacitinib in Patients with Psoriatic Arthritis and Inadequate Response to Biologics: 56-Week Data from the Randomized Controlled Phase 3 SELECT-PsA 2 Study. Rheumatol Ther. 2021 Apr 28. doi: 10.1007/s40744-021-00305-z. Online ahead of print.
- Pipeline – Our Science | AbbVie. AbbVie. 2021. Available at: https://www.abbvie.com/our-science/pipeline.html. Accessed on July 27, 2021.
- A Study to Evaluate Efficacy and Safety of Upadacitinib in Adult Participants With Axial Spondyloarthritis (SELECT AXIS 2). ClinicalTrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04169373. Accessed on July 27, 2021.
- Evaluation of Upadacitinib in Adolescent and Adult Patients With Moderate to Severe Atopic Dermatitis (Eczema) (Measure Up 1). ClinicalTrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/ NCT03569293. Accessed on July 27, 2021.
- A Study of the Efficacy and Safety of Upadacitinib (ABT-494) in Participants With Moderately to Severely Active Crohn's Disease Who Have Inadequately Responded to or Are Intolerant to Biologic Therapy. ClinicalTrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT03345836. Accessed on Accessed on July 27, 2021.
- A Study to Evaluate the Safety and Efficacy of Upadacitinib (ABT-494) for Induction and Maintenance Therapy in Participants With Moderately to Severely Active Ulcerative Colitis (UC). ClinicalTrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT02819635. Accessed on July 27, 2021.
- A Study Comparing Upadacitinib (ABT-494) to Placebo in Adults With Rheumatoid Arthritis on a Stable Dose of Conventional Synthetic Disease-Modifying Antirheumatic Drugs (csDMARDs) Who Have an Inadequate Response to csDMARDs Alone (SELECT-NEXT). ClinicalTrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT02675426. Accessed on July 27, 2021.
- A Study Comparing Upadacitinib (ABT-494) to Placebo and to Adalimumab in Participants With Psoriatic Arthritis Who Have an Inadequate Response to at Least One Non-Biologic Disease Modifying Anti-Rheumatic Drug (SELECT - PsA 1). ClinicalTrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT03104400. Accessed on July 27, 2021.
- A Study to Evaluate the Safety and Efficacy of Upadacitinib in Participants With Giant Cell Arteritis (SELECT-GCA). ClinicalTrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT03725202. Accessed on July 27, 2021.
- A Study to Evaluate the Efficacy and Safety of Upadacitinib in Subjects With Takayasu Arteritis (TAK) (SELECT-TAK). ClinicalTrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04161898. Accessed on July 27, 2021.
SOURCE AbbVie

Related Links
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
Newsrooms &
Influencers
Digital Media
Outlets
Journalists
Opted In






Share this article