Cincinnati Children's Launches Center for Stem Cell and Organoid Medicine
Mission is to Generate Human Organs to Study, Cure Disease
CINCINNATI, Nov. 15, 2017 /PRNewswire-USNewswire/ -- Seven years ago Cincinnati Children's scientists first used pluripotent stem cells to mimic natural human development and grow working human intestine in a lab. Today medical center doctors can bioengineer the gastrointestinal tissues of sick children to find clues about a child's disease and how to treat it.

Cincinnati Children's is building on this early research advancement in personalized medicine by launching the Center for Stem Cell and Organoid Medicine (CuSTOM). The center will accelerate the transfer of stem cell-organoid technology from the research lab to practical clinical tool.
Organoid technology has the potential to solve several current medical and research challenges, according to Aaron Zorn, PhD, the new organoid center's director. The technology gives researchers a first-in-class physiological platform for laboratory research on living diseased tissue, which cannot be done on patients. It can provide laboratory human modeling systems in a petri dish for developing and testing drugs before expensive clinical trials.
Ultimately, the technology can address a shortage of organs available for transplant.
The new center is organized to be a highly collaborative, multi-disciplinary center of excellence that integrates scientists, physicians, geneticists, bioengineers and entrepreneurs, according to Zorn. It is believed to be the first dedicated facility at a pediatric medical center focused on advancing pluripotent stem cell-organoid technology and translating its potential to clinical practice.
"We have this convergence of transformative breakthroughs in organ-generation technology at Cincinnati Children's, and it's critical that we speed up the translation cycle so patients can benefit more quickly," Zorn says. "This is, by definition, personalized medicine."
Foundation of Discovery
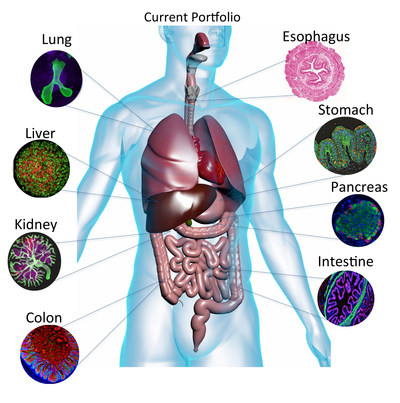
In a series of studies published since 2010, medical center researchers led by developmental biologist James Wells, PhD, the new center's chief scientific officer, used human pluripotent stem cells to bioengineer gastrointestinal tract tissues that mimic natural human development in a laboratory. Scientists tissue engineered the small intestine, colon, stomach, and in a separate study, small intestine with a functioning nervous system. They then used these to study different gastrointestinal diseases.
Medical center researchers also bioengineered mini livers in landmark studies led by Takanori Takebe, MD, a physician and scientist serving as the organoid center's associate director of commercial innovation. Liver organoids hold the nearest-term clinical potential as a personalized platform to test toxicity and efficacy for new drugs, in organoids grown from patients' cells for diseases such as drug-induced liver injury and steatohepatitis.
Cincinnati Children's scientists are also working to bioengineer human esophageal, kidney, lung tissues to study human development and disease.
The lab-bioengineered tissues reveal the precise genetic and biological processes that cause disease, say researchers. Mini organs can identify the unique biological characteristics of a disease in a single person.
The overall effort to study translatable applications for organoid technology is led by Michael Helmrath, MD, the new center's associate director of clinical translation and surgical director of intestinal research and rehabilitation.
One early translational test of stem cell-organoid technology involves Helmrath using donated blood samples from GI patients to generate genetically matched pluripotent stem cells and then biologically recreate that child's intestine to study genetics and biology of his or her disease. Researchers then can use the organoids to test the effectiveness of treatment regimens (nutritional plans, etc.) on the bioengineered intestines.
Science Energized
Cincinnati Children's initial investment in the center is about $13 million, including the cost of earlier research that forms the basis of the center's current stem cell/organoid technology. Working closely with Cincinnati Children's innovation and commercialization office, the center is exploring other capitalization and philanthropic opportunities to expand laboratory facilities and equipment, add scientific staff, and create a translational facility to develop stem cell-organoid systems into commercially-viable products and direct patient care.
The technology accelerator includes these key areas:
- Expand Cincinnati Children's pluripotent stem cell laboratory, where patient-specific stem cell lines are generated and maintained. Fully integrate the use of a precise gene-editing technique known as CRISPR, which can be used to repair genetic defects in the cells of diseased tissues.
- Expand bio-banking activities to increase the number of donated patient clinical samples available for testing and research.
- Enhance existing GMP (good manufacturing practices) facilities at Cincinnati Children's to allow production of clinical-grade human organ tissues that could be used for human transplant.
Translating Research
GI conditions range from simple indigestion to complex conditions like necrotizing colitis or colon cancer. People process oral drugs in the GI tract, making this critical to human health. And research shows that intestinal health is inextricably linked to the immune system and overall health.
To create more opportunities for scientific breakthroughs that have translatable clinical potential, the new stem cell-organoid center strengthens ongoing interdisciplinary cross-collaborations between stem cell scientists and the medical center's dozens of research and medical divisions.
This includes a collaborative team of investigators pursuing a five-year federal grant from the National Institutes of Health focused on generating human organoids that model, study and uncover the genetics of birth defects of the esophagus and trachea.
Although medical center surgeons can surgically repair and reconstruct esophageal and tracheal malformations, these children face a lifetime of chronic health challenges. The center's eventual goal is to grow healthy, genetically matched esophageal and tracheal tissues for regenerative medicine or transplant, says Helmrath.
In his role as the center's chief scientific officer, Wells, a developmental and endocrinology biologist, will help guide the overall scientific focus of the new center as it relates to refining the technology so it can advance to medical practice.
As the organoid center's associate director of commercial innovation, Takebe will help identify organoid center technologies with commercialization potential and then coordinate with Cincinnati Children's technology commercialization staff to find industry collaborators.
These collaborations are critical to facilitate rapid technology translation to the patient care pipeline, center officials said. This includes the ability to conduct high-speed screening of drug libraries in organoids for identifying therapeutic applications, and increased production capacity for clinical-grade human organoid tissues suitable for transplantation.
SOURCE Cincinnati Children's Hospital Medical Center
Related Links
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
Newsrooms &
Influencers
Digital Media
Outlets
Journalists
Opted In






Share this article